In my prior post, I already commented on how programs should downstaff if they are able to. The rationale is that we will experience a high surge in volume, so it is ideal to give staff rest while also using remote hospitalists to working out the kinks in remote clinical roles that you may want to implement when volume surges.
It would be incredibly helpful to get a sense from epidemiologists when the surge is anticipated. Obviously, we all want to flatten the curve and hope that the volume rise will only occur at a slow rate that our healthcare system can safely absorb. But social and other measures may not flatter the curve enough. That means that hospitalist programs need to be prepared for surges.
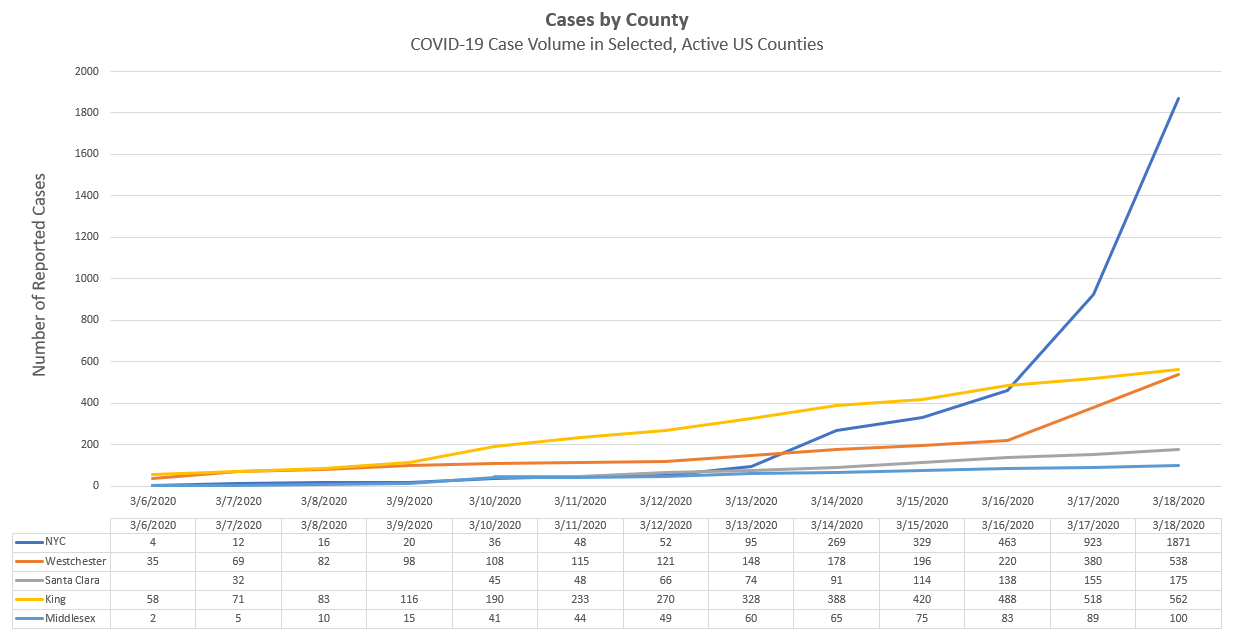
One way to consider volume surges is to look at your local volume. Currently, many agencies (state Department’s of Public Health, the CDC, etc) are only visually representing what is happening state-wide, or even worldwide. The Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) tracks worldwide volume, and the CDC tracks state-based rates of the illness, with some additional information available like breakdown of source of infection, volume by date of infection, etc.
Hospitals and hospitalist programs need to compare local data to date from around the country (or world) which is reported at a local level as well. It is unhelpful for me to evaluate the rate of cases in Washington, compare that to the total case count in Massachusetts, and somehow draw a conclusion. Or, evaluating the rate of rise on the Washington curve, and determining the same slope for Massachusetts, that really is not local-enough data to draw conclusions and make decisions about staffing.
Instead, getting data at least by county would be much more helpful. Through extensive review of news sources and state DPH data, as well as other sources, I was able to compile the graph above (updated as of 3.18.20 data). King County is Washington, where the outbreak spread extensively through the Life Care Center, is now seeing a lot of cases, essentially with significant community transmission. One may think that the rate of rise in Middlesex County, where the Biogen outbreak occurred, may soon match the rate of rise of cases in King County. King County, however, appeared to institute school closures and gathering limitations later, relative to the status of the outbreak, than did Middlesex County (and the state of Massachusetts).
All that said, the Middlesex volume will certainly increase, and clearly no one knows what the rate of rise will look like in Middlesex. Clearly, if the slope of the curve approaches King County, there would be a huge rise in volume within just a few days. What this tells me is that (I hope) we have a few days to prepare for King County like volume. Practically, this means takes several steps. I would suggest taking these steps now – but at the latest you should work through this list when the first COVID patient is positive in your county.
- Discuss with your staff the plan to upstaff the service when volume rises. Tell them to update whatever schedule system you use with the days/nights that they can work. If they have requests off in a scheduling system that are no longer relevant (spring vacation plans cancelled, etc), have them remove those. You need to be able to send a bulletin out to everyone who can work for a particularly day that coverage is needed. Clean this system up now.
- Evaluate remote options for clinical coverage now (cross-cover, triage, virtual visits with patients, etc) and test them out now.
- Plan for roll-out of a remote shift to support non-hospitalists that end up covering your service. This remote shift, which needs to be staffed by a hospitalist, will need to support many types of questions that non-hospitalists that you recruit to cover your service (primary care physicians, specialists, etc). They will have EHR related questions, clinical questions, and system-questions. You can’t ask these providers to work on your team if you can’t support them. Work with hospital leadership now to identify other resources (IT trainers, etc) that may help with some of these functions.
- Work with Medical Staff Leadership to immediately identify physicians and advanced practice providers that can be re-purposed to work on your inpatient hospitalist team. Ensure Medical Staff Leadership and your credentialing department are ready to expand privileges for people, and work through any potential compliance questions that arise.
- Begin to on-board those physicians and APPs now, you won’t have the bandwidth to on-board new providers when volume surges.
- For a first wave, I would suggest on-boarding at least 100% of the rounding hospitalist teams that you depend on every day. This rule of thumb provides a reasonable start to provide you with coverage to staff those teams if hospitalists become ill; you can also use these staff to help with evening and nights. For example, if you have 8 rounding teams and 2 physicians at night along with 1 PA at night, on-board at least 8 people now.
- Within 24 hours, continue expand your pool of clinicians, but now focus on medical consultants and discuss with them transitioning to an attending role for patients admitted primarily with problems related to their specialty area. This will free up your staff to care for COVID patients and other patients that are admitted. Make them aware that you will work together to make this work! You will have remote hospitalist support available for questions that arise regarding clinical issues that are not in their specialty area.
In my posts tomorrow, I will review
- Surge planning for volume with more granularity
- Will provide several clinical tip sheets for COVID-19 that have been completed (and link to some wonderful resources put out by Hopkins and others related to these topics)
- Will post some important resources you need to be aware of regarding ventilator allocation should disaster volume be realized.


[…] Hospitalist Service Staffing […]