Estimating increases in volume as COVID-19 increases in your community is obviously not an exact science. There is, however, a wealth of emergency preparedness information available in general, and using these resources to make some estimates will be necessary. By using a model, you can then apply volume estimates to your service, and make decisions about staffing for your service. Unfortunately, there does not appear to be much guidance regarding best practices at the level of your service. That is, best practices related to surge planning, adapting workspaces, planning for expansion of ICU beds, and re-purposing personnel do not give you any model or formula to guide staffing changes.
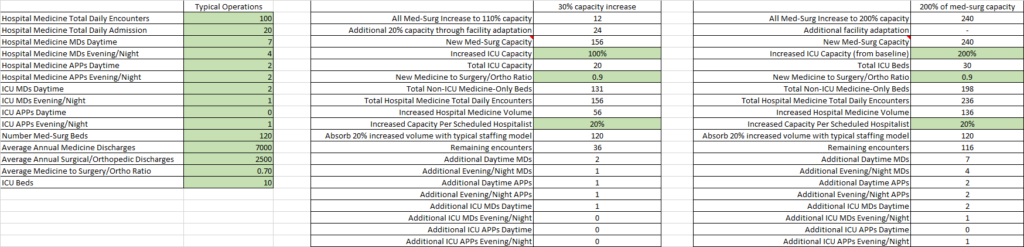
To create a model for surging your own service’s staffing, one needs to make some assumptions about your hospital’s surge capacity, how much each of your hospitalists will increase their daily visits (if at all), to what extent the ICU will surge into Med-Surg beds and other areas. By makes these and other assumptions, you can then take data from your own program and model volume increases. Of course, it will be necessary to run different models, as volume may surge more rapidly that expected (requiring that you move to a higher volume model right out of the gates), and also because, if the COVID-19 case volume rise is successfully blunted, different models may need to be implemented sequentially.
With respect to making assumptions about surging, data from hospitals that experienced disasters (9/11, Katrina, mass shootings) provides some insight into how hospitals should be expected to surge. I found this guidance from the Johns Hopkins Bloomberg School of Public Health particularly helpful. In their recommendations, they state the following:
- Be able to make 30% of licensed bed capacity available for COVID-19 patients on 1 week’s notice. About 10-20% of a hospital’s bed capacity can be mobilized within a few hours by expediting discharges, using discharge holding areas, converting single rooms to double rooms, and opening closed areas, if staffing is available. Another 10% can be obtained within a few days by converting flat spaces, such as lobbies, waiting areas, and classrooms.
- Collaborate in regional plans to be able to make at least 200% of licensed bed capacity in the region available for COVID-19 patients on 2 weeks’ notice.
The Institute of Medicine’s 2012 report titled “Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response” also provides some very helpful guidance, which basically indicates that surge capabilities vary considerably from hospital-to-hospital.
Each hospital should have concrete goals for expansion during a disaster, including outpatient, inpatient, and specialty unit capacity. However, the extent to which a hospital can surge will vary. Recommendations are not standardized; for example, Israeli hospitals are required by the government to be able to increase their capacity by 20 percent within hours (Peleg and Kellermann, 2009), while a U.S. critical care workgroup recommended surge capacity of 200 percent over usual intensive care capacity (Rubinson et al., 2008a), which would involve significant operational planning (Gomersall et al., 2006; Hota et al., 2010; Rubinson et al., 2005). The role of the institution in the community and its size contribute to this calculus. For example, it may be easier for a smaller hospital to surge to 200 percent of a small number of critical care beds, and a higher goal may be in order (as compared with a tertiary hospital). Similarly, a level 1 trauma hospital with an accredited burn unit will be expected to be prepared for a much larger number of operative and burn patients than a hospital that does not usually receive trauma cases. A consensus group has recommended that pediatric intensive care units be prepared to provide 100 percent surge capacity (doubled volume) for 10 days (Bohn et al., 2011).
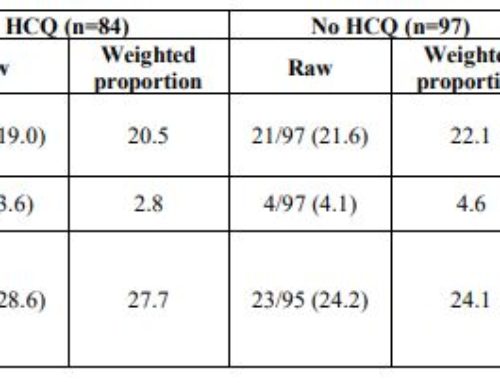
Literature to support these levels of increases was also supported from other literature, including this publication from just a short time prior to the start of COVID-19 illness.
As previously reviewed, the rate of COVID-19 case increases vary considerably by county. Remember that using your LOCAL data to estimate when you may surge is most helpful (as opposed to state volume, etc). When the slope of your county curve begins to increase, or when you begin to experience a significant rise in volume irrespective of what is being reported in the county, I would suggest implementing staffing increases to accommodate a 30% increase in bed capacity within 1 week, which can probably be considered the first surge level, as per the above-noted recommendations. Recognizing the the curve can rise rapidly, put plans in place when the curve does begin to rise. Do not wait until you are experiencing substantial surge volume.
A 30% increase in bed capacity DOES NOT equate to a 30% rise in Hospital Medicine volume. In order to next determine the rise in Hospital Medicine volume, one needs to consider the number of licensed med-surg beds, and then make assumptions about how those beds, and any additional beds, will be utilized. Given elective surgeries will be cancelled when we reach this first surge level, a large proportion of beds that are typically occupied by elective surgical/orthopedic patients will now become hospital medicine beds. Further, this first surge level will need to expand ICU beds, which may be expanded into conventional med-surg spaces. To calculate the number of beds hospital medicine will actually be staffing in a COVID-19 surge, the new proportion of licensed med-surg beds that will be cared for by hospital medicine needs to be determined, and one must then add to that a 30% increase in beds (again subtracting any small proportion of orthopedic/surgical volume), and then subtracting med-surg beds that are converted for ICU care.
Taking an example, if a hospital has 100 licensed med-surg beds, it should expect to increase to 30% perhaps within a week from when the COVID-19 curve begins to rise in your county. To keep things simple, assume that occupancy is 100% and that hospital medicine cares for all medical patients in the hospital. Conventionally, assume that of the 100 med-surg beds, this hospital has 50% medicine and 50% surgery. This means that hospital medicine has an average daily census of 50 patients. With COVID-19 ramping up, assume that the medicine and surgery capacity shifts, such that medicine is now 90% of beds. That means that hospital medicine now has an average daily census of 90 patients per day. That is BEFORE you even surge from your licensed bed capacity. If you now increase to 130 beds, assuming medicine is responsible for 90% of those extra 30 beds, that means that hospital medicine bed capacity increases to 117. If this hospital has 10 ICU beds, it is probably reasonable to assume that this capacity will need to double with this first surge. Therefore, 10 med-surg beds would need to be utilized for ICU, which means hospital medicine (assuming hospitalists are not caring for ICU patients) now are down to 107 beds.
By making assumption about length of stay, and tallying your total daily daytime and evening/overnight hospitalists, you can then use these volume estimates to determine the number encounters per day, and how many extra staff you will need. When taking the volume estimates and determining staffing needs, one needs to consider if they will increase the volume of each existing hospitalist. That is, if a rounder usually sees 15 patients in a day, is your goal to maintain that number of daily encounters? Probably not, since increasing encounters per day per hospitalist will limit the staffing surge you will require while limiting staff exposures, enhancing staff social distancing, and since you will probably also put other supports (such as remote hospitalist APPs) into play to help support the on-service hospitalists.
Using this type of model, estimates of volume increases and required staffing increases can be made. A similar model for hospital medicine volume and corresponding required staffing increases can be applied to the next surge, where hospital capacity increases 100% from usual licensed med-surg beds. A snapshot from an Excel Spreadsheet where you complete the fields in green is below. It is completed with numbers from a fictional program, just to give you a sense for how it works. I am trying to figure out how to make this available for download, but feel free to contact me for now and I will send it to you.
Based on this model, this hospitalist service would need to go from 7 daytime MDs to 9 daytime MDs, and from 4 to 5 evening/overnight MDs. Estimating the increases needed and making assumptions about the percent of your staff that will be out due to viral respiratory illnesses, you will need to plan to bring on others to join your team ASAP, as discussed in greater depth in my prior post on staffing.


[…] Estimating Surge Volume […]