In my prior post, Crisis Standards of Care #1, I reviewed the Crisis Standards of Care framework in general. Page 1-82 of the IOM Crisis Standards of Care (CSC) report, which pertains to the Sixth Standard, Palliative Care, including this following information:
A triage system for allocation of scarce resources will function best if it is transparent; fair; valid; consistent across settings and events; dynamic (applied at multiple places and times); and flexible enough to address changing circumstances, including responding when patients triaged as likely to die actually improve or when additional treatment resources become available (Matzo et al., 2009). Preserving a functioning health care system during and after a disaster will require the adoption of principles of field triage, limits on the use of ventilators and surgery, and the creation of alternate care sites. Research is beginning to provide a scientific underpinning for triage (Sacco et al., 2005), as well as to identify basic criteria for critical care triage during a disaster in which medical resources are scarce (Devereaux et al., 2008; Wilkinson et al., 2007). Future research will have to address the applicability of triage to palliative care, as well as the role of palliative care in disaster response. The arguments for incorporating palliative care into disaster response—humane treatment, diversion of dying people away from overburdened hospitals, more effective use of scarce resources, and the provision of care that patients want—have moral weight on their own, but research should still assess their impact.
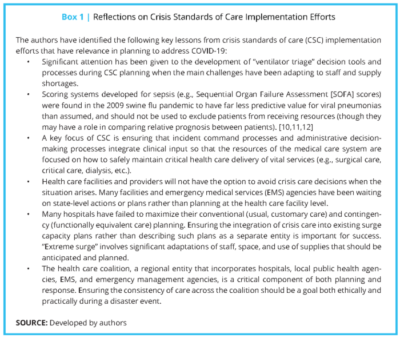
Since 2012 when these standards were published, additional crises have occurred, which provided an opportunity to learn from these standards and refine them. A group of experts convened on 11/21 to discuss what we have learned about the Crisis Standards of Care in the last decade. While I am unable to find any report from that workshop, a post put out by the National Academy of Sciences As detailed by the National Academy of Sciences provides some critical lessons about emergency management.
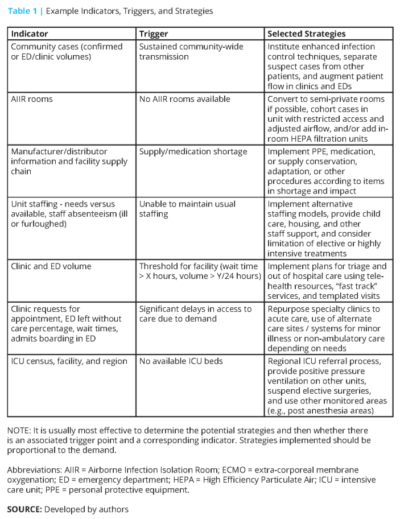
In their blog post, the authors share a multitude of helpful strategies to deal with some of the greatest challenges that we either are facing now or make be addressing soon. They discuss best practices for staffing, the importance of child care for healthcare workers, key elements of an inpatient surge plan, and ICU surge as well. They further post three tables which I found particularly helpful, two which I pasted here:
The authors note that their lessons learned include the need for an emphasis on adapting to staffing and supply shortages, rather than as much effort necessarily on ventilator triage protocols. That reminds us all that if we plan for staffing optimization now, and if we are creative in the ways that we leverage all of the members of our committed, collective medical staff, we will be best prepared to care for escalating numbers of patients.
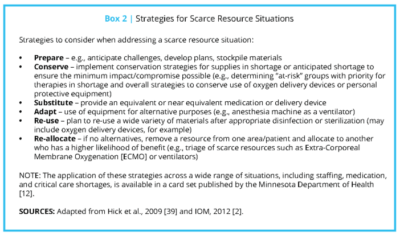
Despite the best preparation, there are significant concerns that we will be facing supply shortages at a national level. Shortages not only involve very scarce resources (such as ventilators and ECMO equipment), but also common resources where scarcity would never cross our mind. These may include endotracheal tubs, surgical masks, eye protection, contact precaution gowns, medications, and other supplies. Consider now, alongside your hospital leadership and directors of Materials Management, what your supply chain looks like. What orders are expected to come in and how much do you have on hand? Clinicians, along with hospital leadership, should be involved in decision-making about reuse, and if reuse is institute, on the duration of reuse. Reuse may mean 1 day now, but may mean 2-3 days, or longer, in the future. Plan now, plan now, plan now. You do not want to be arriving to admit another sick patient with suspected COVID only to find the precaution cart is empty, with no supplies to be found on the unit or other units in the hospital. See below for another table from the authors which provides some examples of how to deal with limited capacity to address all of the needs that are anticipated to arise.
In the same vane, please plan now, alongside your critical care, palliative care, and anesthesia colleagues a process for ventilator utilization. When considering “ventilator triage” protocols, please take time to review the authors perspectives on this, which I think are critical.


[…] Crisis Standards of Care #2 […]