Many people have begun to ask about making their own PPE. I know there are many examples on social media of this, with pictures and even methods to do this.
There is not data on specifically how different materials and home made masks protect against coronavirus, neighter the prior SARS and MERS nor the current COVID-19. There is some interesting data on how different materials may hold up when re-purposed as surgical mask materials. My wife is very handy, and is interested in making masks out of available materials. To effectively make a surgical mask that can hold up and remain free of defects, she tells me that you would ideally use a surger machine as opposed to a sewing machine.
When considering using any homemade materials, you need to first work with your infection control experts to discuss implementing this. Reuse of PPE in general is not the norm, and using homemade masks is certainly not conventional either. However even infection control experts would agree that it is better to wear some protection than no protection. When the time comes that your facility begins to run low on PPE, and they implement policies for reuse as well as extended use, following that your infection control leaders may endorse certain homemade PPE, specifically masks. Think about options now for homemade PPE – instead of everyone creating their own version of what they think is most protective and their own policy for reuse and extended use, and cleaning, it is better to plan now with your infection control experts so that when you need homemade PPE. Planning use around homemade PPE will create some basic standards, such as materials that are recommended, how and if to wash, minimum standards for craftmanship, etc.
First and foremost, we need to accept that there are areas in the world and county now where people are doing this. The CDC should provide guidance NOW regarding homemade masks, as people invest effort into this and make their own PPE. If we do not get guidance soon, healthcare workers may be placed at an unnecessarily high risk because they are using the wrong materials, following inappropriate sanitizing procedures, etc.
Some information on materials and a discussion about what people are doing can be found at this Hospitalist article. They refer to an interesting publication from 2008 from PLoS One. In this publication, the authors conclude:
It is also clear that home-made masks such as teacloths may still confer a significant degree of protection, albeit less strong than surgical masks or FFP2 masks. Home made masks however would not suffer from limited supplies, and would not need additional resources to provide at large scale. Home made masks, and to a lesser degree surgical masks, are unlikely to confer much protection against transmission of small particles like droplet nuclei, but as the reproduction number of influenza may not be very high [14] a small reduction in transmissibility of the virus may be sufficient for reducing the reproduction number to a value smaller than 1 and thus extinguishing the epidemic [15]. Greater reduction in transmissibility may be achieved if transmission is predominantly carried by larger droplets. In a typical human cough half of the droplets may be small (<10 µm), but these comprise only a small fraction (2.5*10−6) of the expelled volume [12].
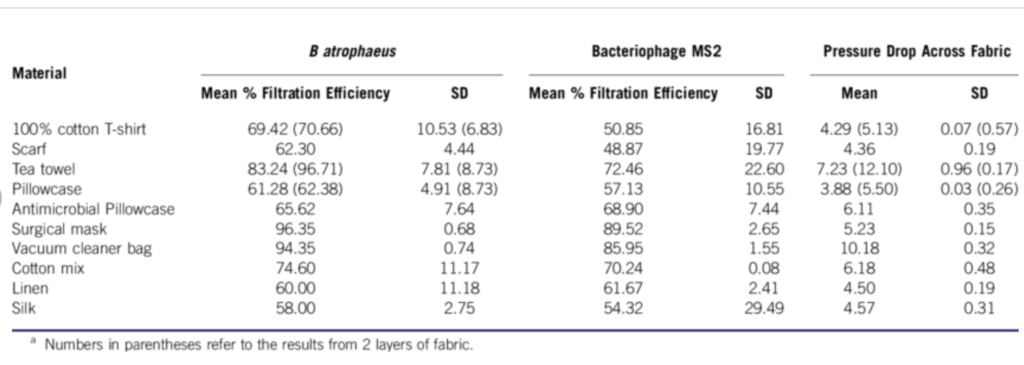
Another study from Disaster Medicine and Public Health Preparedness from 2013 actually tested a variety of household materials to see how they fared against high concentrations of bacterial and viral aerosols to assess their filtration efficiencies. Below are the results of how each material fared.
Keep in mind that these results are not specific for COVID-19, but it is what we have so worthwhile to review.


Leave A Comment