While we hope for the curve to flatten, we need to be prepared for a crisis situation where hospital beds become a precious commodity and where ventilators are in short supply. Such a situation means that difficult decisions need to be made. Hospitalists cannot be left alone to make these decisions. Collaborating with leadership from your Ethics/Complex Care Committee, ED, intensive care unit, palliative care service, anesthesia, and your legal resources will be critical and needs to happen now. By planning now, and working with these constituents to develop a rational policy which is based on the best information we have on outcomes for COVID specifically and also based on experience with prior crisis situations, hospitalists and other providers will not be put in the extremely uncomfortable and ethically reprehensible position of making decisions on an ad hoc bases. These principles are perhaps best put by experts in emergency management, including Dr. Kick and Wynia:
It is unfair, inefficient, and potentially cruel, so the thinking went, to leave clinicians to make ad hoc rationing choices during an epidemic without good guidance, support, and protection. Given that, a major purpose of crisis standards of care protocols is to support clinicians and planners across a spectrum of care, including extreme cases in which clinicians could be forced to choose who lives and who dies.
Guidance for clinical triage should optimize survival across a population by translating the best available evidence into reliable algorithms that can be used at the point of care. The ethical justification generally given for withholding or removing potentially lifesaving care from one person or group without their consent and giving it to another is that the latter person or group has a significantly better chance at long-term survival.
The authors go on to review that we need data in order to make these decisions based on facts:
Yet the 2009 National Academies report recognized that triage decision aids of the time were primitive, simplistic, and mostly untested for use in disasters. Today, clinical triage guidance specific to Covid-19 is urgently needed. Real-time clinical data should be used to develop an accurate, predictive model for death due to this disease. We need to know who is most likely to survive if they are given a full-court press and who is most likely to die regardless of treatment.
All that said, and as I pointed out above, we need standards now. That is not to say that we can’t adjust such standards as we develop a better understanding of how co-morbidities and factors related to the condition itself impact, but we need to plan now. There is a body of literature on this subject. This publication (published in 2011) specifically addresses the need for a pandemic rationing and appeals process. If you are interested in prior research looking at the number of ventilators needed during a pandemic, check this publication out from IDSA in 2015 (full text available). Just to summarize a key point, with an estimate of a 30% clinical attack rate (much lower than that of COVID-19 estimates), and assuming a case-fatality rate of 0.25%–0.5% (also much lower than we think for COVID-19), in the authors estimated that we would require 35,000 to 60,500 additional ventilators, averting a pandemic total 178,000 to 308,000 deaths.
In any event, I hope the experts in emergency preparedness and the epidemiologists who modeled the impact of a pandemic have convinced you that a triage plan is needed now. I think it is obvious that you should not wait to do this. If you need any more convincing, please see this Perspective in NEJM published on March 18th, 2020. The publication, titled “Facing Covid-19 in Italy — Ethics, Logistics, and Therapeutics on the Epidemic’s Front Line” is a gut-wrenching reminder that we really need to be thoughtful about this now. It would be inexcusable to leave this to a front line ED doc, hospitalist, or intensivist to try to improvise such gravely consequential choices.
While it may seem overwhelming to consider such a plan for several reasons, the burden is relieved when you realize that you don’t need to start from scratch. Our colleagues in the field of emergency preparedness have also considering this, and provide some wonderful guidance. These triage protocols are based heavily in several ethical principles, which may include beneficence, fairness, utility, accountability, transparency, proportionality, reciprocity, distributive justice and stewardship. For some additional information regarding these principles as they relate to ventilator triage, see pages 17-18 of this approach to ventilator allocation published by the State of Michigan Department of Community Health Office of Public Health Preparedness. (The publication from 2012 also provides information about federal legal protections on pages 81 to 82). In that publication, it is interesting that Michigan espoused utility (prioritizing ventilators for physicians, nurses, etc), but there are clearly ethical arguments why that could be a reasonable approach.
The New York State Task Force on Life and the Law published its “Ventilator Allocation Guidelines” in 2015, and provides a comprehensive approach to triage guidelines. This system, and others I have seen, starts with exclusion criteria, and move into triaging patients into priority categories. Interesting, in contrast the Michigan protocol, the New York guidelines do not incorporate utility into their algorithm (i.e. do not prioritize doctors, nurses, etc). They provide rationale for that decision in pages 44-45 of their report, which brings us on a bit of a tangent but which I think is interesting to share here, given the general audience:
Upon reexamination of this issue, the Task Force confirmed that patients should be assessed on medical factors only, regardless of their occupation. In a pandemic, if a health care
worker with influenza needs ventilator therapy, s/he will be unlikely to return to work or care for patients. Thus, the argument that these individuals should receive priority access to ventilators so that they may continue to treat patients is moot. Second, workers in many occupations risk exposure and provide crucial services in a pandemic. Doctors and nurses face risks, but so do respiratory therapists, orderlies who keep rooms clean, morgue workers, laundry workers, ambulance staff, security personnel, fire fighters, police, and others. Nor is it always easy to determine who is a health care worker. Part-time volunteers staff ambulances in some communities; and an unpaid family member may serve as the full-time caregiver for a disabled relative. These unpaid providers take risks comparable to or greater than some paid health care providers. Expanding the category of privilege to include all the workers listed above may mean that only health care workers obtain access to ventilators in certain communities. This approach may leave no ventilators for community members, including children; this alternative was unacceptable to the Task Force. The 2006 Adult Clinical Workgroup also objected strongly to the appearance of favoritism, in which those who devised the clinical ventilator allocation protocol appeared to reserve special access for themselves. Thus, the Task Force reaffirmed the Workgroup’s conclusion that access to ventilators should depend on clinical factors only.
The New York algorithm does not directly incorporate age, which is clearly debated and something that is already in use elsewhere where COVID-19 is overwhelming the healthcare system (Italy most notably at the time of this post, although this is based primarily on several anecdotal reports). The publication from New York provides the following rationale for the decision not to include age:
However, the Task Force believed that to exclude older adults discriminates against the elderly, especially where there is a greater likelihood that the advanced-aged patient will survive.
Because age already factors indirectly into any criteria that assess the overall health of an individual (because the likelihood of having chronic medical conditions increases with age), the Task Force affirmed that the use of advanced age as a stand-alone triage factor should be rejected.
The New York criteria are listed here:
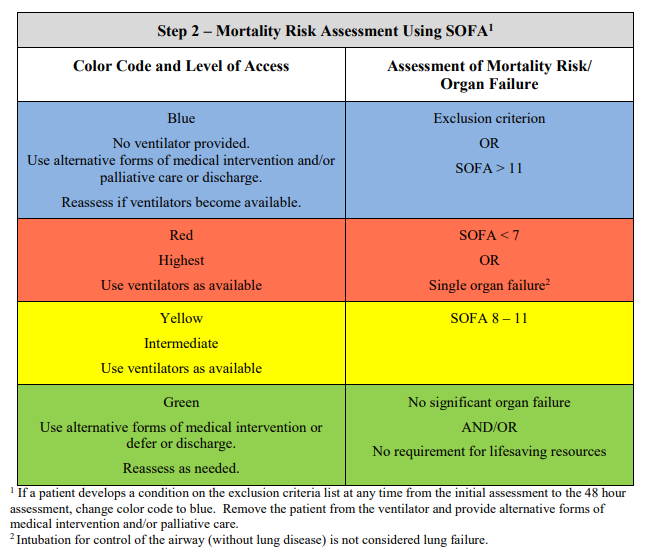
Following application of the exclusion criteria, the guidelines deploy “Step 2” which is a Mortality Risk Assessment Tool. Various scoring systems are obviously out there, but it appears that the one most espoused for purposes of ventilator allocation strategies is the SOFA score. The Step 2 of the New York algorithm then uses the SOFA to stratify patients into different colors, which then prioritize ventilator allocation. Reassessments of patients at 48 and 120 hours using a color-coded prioritization scheme is them deployed. The first assessment (on presentation) is reviewed here:
An example of a triage algorithm that does incorporate age, along with many other exclusion factors (making the algorithm somewhat more complex), can be reviewed in this Canadian Medical Association Journal publication.
All algorithms do have in common establishing a triage team that is responsible for considering the patient in the context of the exclusion criteria, risk assessment framework, and overall guidelines. Establish the membership of these teams now, and this team can serve on your planning committee to develop and endorse these guidelines. These available algorithms also incorporate procedures for considering when to extubate someone who is not progressing well. This last point is of particular debate with COVID-19, since it is well-described that the duration that patients require ventilator support is long, and the duration therefore is not necessarily a predictor of poor outcome. Also, there is some sense that SOFA may be a poor predictor in patients with viral pneumonia (was not a great mortality predictor in SARS and MERS), however there is not a better tool necessarily for prediction of mortality in patients with viral pneumonia, so reasonable to use the SOFA for now.
Two final points to consider. It is recommended that any algorithmic approach (or at least guideline) for ventilator allocation is implemented ideally at the state level – however there may not be time for this and so getting your health system harmonized with your hospital’s strategy will be an important first goal. Consider the issues that would arise if several hospitals in the same geographic service area had drastically different ventilator allocation rules – those implications can be discussed by the ethicists.
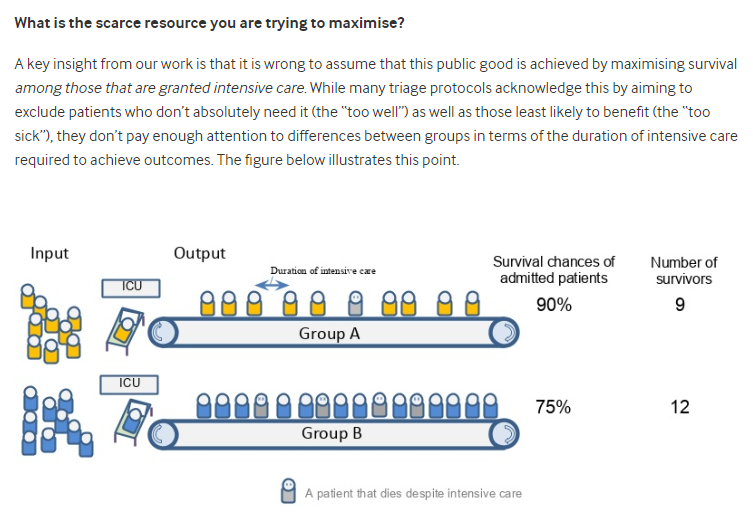
Lastly, I will leave you with this fascinating insight from BMJ titled “Covid-19: How to triage effectively in a pandemic. This thoughtful opinion piece makes it clear how very complex this topic is.



[…] this challenging time, hospitals and states are developing ventilator triage guidelines in accordance with carefully consid…. The chaotic circumstances that will naturally occur during any time when ventilator triage even […]